Report: Neurodivergence and substance use
This report investigates the connection between neurodivergent conditions, specifically attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD), and substance use.
We explore the research on this topic and provide a literature summary on substance use and addiction in neurodivergent people. Further, through engagement with people with living experience, we explore the perspectives of neurodivergent people who use substances in Aotearoa New Zealand. This report illustrates the complex nature of the coexistence of neurodivergence and substance use, and the difficulties of, and barriers to, seeking treatment in Aotearoa New Zealand.
This report finds that neurodivergence impacts the way in which people engage in substance use in a variety of ways. People with ADHD and/or ASD may be more likely to engage in problematic substance use and to use substances to manage symptoms of their neurodivergence. Interventions targeted towards neurodivergent people who use drugs, particularly those focused on screening for ADHD and ASD, treatment and psychosocial support are imperative for mitigating the risks associated with substance use and self-medication. Stigma, both experienced and perceived, cost and limited access to resources are barriers to neurodivergent people seeking support.
This report is split into three sections: a literature summary, a summary of themes from living-experience perspectives on ADHD/ASD and substance use, and recommendations.
Jump to:
| Literature summary | Community experiences |
| Neurodivergence | Our process |
| ADHD and substance use | Findings and insights |
| ASD and substance use | Recommendations |
| Neurodivergence and substance use in Aotearoa |
Acknowledgements
This report focuses on communities of people who use drugs (PWUD) that are likely to experience compounded stigma as a result of both their drug use and their neurodivergence. People with ADHD, ASD and other neurodivergences often experience societal ostracisation, stigma, and reduced access to health and social services. Our systems, approaches and services in Aotearoa New Zealand are not developed with neurodivergent people in mind. All of these factors complicate the experience of neurodivergent PWUD navigating the world.
Importantly, we want to acknowledge that this report takes a humanistic approach to examining the relationship between neurodivergence and substance use. We underscore the importance of asserting that neurodivergence is not a deficit, rather a biological difference in the brain that affects the way people perceive, experience and navigate the world around them. We take a non-judgmental approach to substance use and acknowledge that people — both neurodivergent and neurotypical, use substances for a variety of reasons.
This report approaches this topic with manaakitanga and upholds the harm reduction values of Te Puna Whakaiti Pāmamae Kai Whakapiri. Most importantly, we aim to uplift the dignity of PWUD and neurodivergent people. We hope that this report promotes understanding of the complexities of this topic and offers a starting place for Aotearoa New Zealand to make changes that positively impact neurodivergent people in their ability to live long, healthy and happy lives.
Finally, we recognise the multifaceted identities of many neurodivergent PWUD. There has been a significant deficit in research and understanding of the relationship between neurodivergence and substance use in Māori and other indigenous peoples, people of colour and ethnic minorities, disabled people, women and the LGBTQIA+ community. As such, this report acknowledges that much of the evidence presented in our literature summary does not reflect the unique experiences of these groups. We hope to see future research provide better insight into the unique experiences of people from an intersectional lens.
Literature summary
Aotearoa New Zealand has faced persistent issues of stimulant drug use (particularly methamphetamine), and comparatively high rates of undiagnosed and untreated neurodivergent conditions, including ADHD and ASD. International literature has illustrated the connection between neurodivergence and substance use; namely, the increased harm from substances experienced by neurodivergent individuals.
Despite this, little has been done to explore the nuances of the specific relationships between substance use, substance use disorders (SUD), and ADHD and ASD, respectively. The group of most interest for this report is people who use drugs (PWUD) who meet the diagnostic criteria for ADHD or ASD but have not received a formal diagnosis.
This literature summary is focused on reviewing a wide variety of research to assess what is known about the relationship between ADHD, ASD and substance use. This section aims to outline the implications and applications of the available research on this topic and to better illustrate the gaps that need to be addressed in future research.
Much of the available research on this topic has been done in the context of treatment settings. Almost all of this research has been conducted outside of New Zealand. Further, research has relied on studying people with diagnosed ADHD and ASD. This is understandable, given the difficulties in accessing individuals who have not been formally diagnosed. However, as a result, it is difficult to draw conclusions about this group from the available research.
Neurodivergence
What is neurodivergence?
Neurodivergence, or neurodiversity, refers to differences in cognition from typical functioning in areas such as socialisation, learning, attention and mood. Neurodivergence encompasses an array of conditions such as ADHD, autism spectrum disorders, fetal alcohol syndrome, dyslexia and dyspraxia. By some definitions, neurodivergence can also include people with diversity in behaviour and mood, including anxiety, depression, obsessive compulsive disorder (OCD) and personality disorders.
For the purpose of this literature summary, we focused on a narrower definition of neurodivergence; specifically examining the relationship between substance use/SUD and ADHD and ASD. However, we acknowledge that there are a significant number of conditions and diagnoses that exclude people from being considered ‘neurotypical’. In future, we hope to broaden our scope to understanding the nuances of other neurodivergence and substance use.
Overall, there is a small body of research that focuses on neurodivergence and general substance use. Most of the literature focuses specifically on ADHD or ASD in individuals with diagnosed SUD. In fact, in our literature scan, we could not find any meta-analysis examining neurodivergence and substance use as a complete topic.
ADHD and substance use
What is ADHD?
Attention-deficit/hyperactivity disorder (ADHD), is a neurodevelopmental disorder that is generally characterised by impairments in attention, and/or hyperactivity and impulsivity.1 ADHD is considered a developmental disorder as it is often diagnosed in childhood. Individual experiences of ADHD differ from person to person. People with ADHD can experience different symptoms at differing severities. ADHD can present as inattentive, hyperactive or a combination of both.2 Inattentive symptoms of ADHD affect a person’s ability to focus and sustain attention on tasks. Hyperactive presentations of ADHD manifest in restlessness, agitation and inappropriately high levels of activity. People with ADHD may also exhibit difficulty with impulse control, have impulsive emotions and experience ‘executive dysfunction’, which results in difficulty organising thoughts, planning and conceptualising time.
Internationally, there is a considerable amount of research on ADHD and its connection with SUD and addiction. However, there is still much that is unknown and undocumented about this relationship. Specifically, there is a massive deficit in research on substance use and ADHD in women, indigenous people and people of colour, disabled peoples and those diagnosed in adulthood.
Aroreretini is a Māori word used in reference to having ADHD. Its accepted translation is “attention goes to many things."
Research shows that people with ADHD are more likely to have used drugs or nicotine across their lifetime, compared to neurotypical people. Childhood ADHD symptoms are also a predictor of subsequent illicit drug use in a person’s lifetime.3 People experiencing worsening ADHD symptoms in their adolescence are also more likely to experience early onset of illicit drug use.4 Early engagement in illicit substance use for people with ADHD is a predictor for escalating substance use, and sustained substance use in adulthood. It also increases the risk of substance use becoming problematic.5
The reasons why people with ADHD are more likely to engage in illicit drug use have been theorised in research. Illicit drug use may stem from self-medication, behavioural disinhibition, impulsivity or sensation seeking, to name some posited ideas.6 However, there is no one single mechanism that can explain the link between ADHD and drug use behaviours.7
Given that over 50% of people with childhood ADHD experience symptoms persisting into adulthood, it is likely that risky or problematic substance use behaviours initiated in a person’s early life may persist for many people with ADHD.8 Despite not fully understanding this complex relationship, we know that ADHD has also been linked to other impulsive and addictive behaviours, including gambling and cigarette smoking.9,10 There is limited literature focused on substance use initiation, or general substance use in people with ADHD. The majority of research is focused on problematic substance use and SUD. This may be a result of the high incidence of SUD in people with ADHD.
Research suggests that about one in five people in the United States with SUD have a comorbid diagnosis of ADHD.11 Other research has posited that over 50% of adults who have ADHD will meet the criteria for SUD at some point in their lives.12 This is a considerably higher proportion than that of neurotypical individuals, which is often cited as between 5–15%.13,14 This rate is also high compared to national figures. In New Zealand, 2006 data estimated the lifetime prevalence of SUD across the population was around 12.3%.15
Childhood ADHD diagnoses have been noted as an established risk factor for the development of SUD in adulthood. Wilens and Biederman (2005) conducted a meta-analysis of this topic in the literature and found a consensus that ADHD is an antecedent disorder for SUD for children and adolescents.16 Overall, there is considerable evidence for a correlation between ADHD diagnosis and SUD across the lifetime; however, these are cases where diagnosis occurs early in life. The relationship between ADHD and SUD is less explored for adulthood diagnoses.
People with ADHD are more likely to have severe or complex SUD, and greater difficulty in responding to alcohol and drug interventions. Research has found that adulthood ADHD was associated with higher SUD severity, polysubstance use and psychopathological complexities.17 People with ADHD are also more likely to experience concurrent SUDs involving addiction to more than one drug.18 This further increases their risk of harm and overdose death.
The reasons why people with ADHD are more likely to experience SUD and complex SUD are not well understood. Some research suggests that the link between the two may be related to shared genetic features between ADHD and SUD.19 Other research has suggested that it could be partially explained by the dysregulation of dopaminergic circuits.20 One prevalent theory is that SUD in people with ADHD could be a product of self-medication, particularly for individuals not receiving adequate diagnosis and/or treatment.21
For a long time, there has been a suggested link between ADHD and illicit stimulant use (e.g., methamphetamine, cocaine). Research has found that ADHD is 2–6 times more common in people who use methamphetamine compared to those who don’t.22 The relationship between undiagnosed ADHD and methamphetamine use in particular has been explored in literature. A 2018 study found that over 10% of people using methamphetamine met the diagnostic criteria for ADHD.23 Undiagnosed and unmanaged ADHD is likely to contribute to regular methamphetamine use. One study of 269 people who regularly used illicit stimulants found that 45% screened positive for adult ADHD.24
People with ADHD are also more likely to experience more severe effects of stimulant substance use on their daily functioning. Studies by both Bordoloi and Chandrashekar and Obermiet et al. showed that ADHD among people classified as “chronic methamphetamine users” increased the frequency, persistence and adverse effects on everyday functioning. They reported a lifetime prevalence of ADHD in 20.8% of “chronic methamphetamine users.”25, 26
Predictably, ADHD is also a risk factor for early onset of stimulant SUD, and consequent harm from these drugs. Adults with ADHD have a more prolonged course and severity of stimulant SUD. Research has also found that the treatment of ADHD alone is insufficient in most ADHD adults with stimulant SUD. Jaffe et al. also concluded that people who used methamphetamine and had ADHD were more likely to leave treatment early and have greater medication non-compliance than those without ADHD.27 People with ADHD symptomology experiencing stimulant SUD also show higher rates of poor functional capacity, higher rates of unemployment and significantly higher neurocognitive symptoms than people using methamphetamine/other illicit stimulants that do not have ADHD.
One theory of why people with ADHD are at increased risk of stimulant use is that these drugs mediate many of the debilitating symptoms of unmanaged ADHD.28 Drugs such as methamphetamine, amphetamine and cocaine act as modulators in similar ways to prescription psychostimulant treatment (i.e., methylphenidate) for ADHD symptoms. Whilst there are still considerable gaps in knowledge regarding self-medication for ADHD symptoms in those without formal diagnosis, this concept is supported by pharmacological perspectives.29 People with ADHD have atypical action of neurotransmitters as well as structural differences in the brain.30 Stimulant medications modulate noradrenaline and dopamine, which help the brain of a person with ADHD to work more ‘typically’. These medications improve focus, memory, executive function and reduce the impact of hyperactivity. Illicit stimulants such as methamphetamine, amphetamine and cocaine have very similar mechanisms of action to prescription psychostimulants and are likely to provide similar relief of some symptoms of ADHD.31
As people with ADHD are far more likely to meet the diagnostic criteria for SUD compared to the neurotypical population, it is reasonable to assume that individuals may also be at increased risk of SUD for non-stimulant substances such as opioids, cannabis or alcohol.
In a study of people with opioid use disorder (OUD), the prevalence of ADHD among patients undergoing opioid maintenance treatment was 20.3%.32 This is considerably higher compared to the general adult ADHD prevalence, at around 2%.33 The study found that over 83% of individuals who had ADHD and OUD had not been diagnosed prior to the study. As with other substances, it can be speculated that opioids may be used by people with ADHD to help modulate symptoms, especially if a person is not receiving ADHD treatment.34
Research has been done to investigate the link between ADHD and regular cannabis use. People with ADHD are more likely to report cannabis use compared to the general population.35 Research has suggested that regular cannabis use may function as a way of managing symptoms and reducing executive dysfunction associated with ADHD. Cannabis may also help to mitigate the effects of pharmacological treatment for ADHD, such as difficulty sleeping and reduced appetite.29 Research has also shown that individuals with self-diagnosed ADHD may also opt for cannabis as a treatment for ADHD symptoms rather than seeking traditional stimulant medication.36 Similarly, an analysis of online forum discussions of ADHD and cannabis use found that there was a large contingent of people suggesting that regular cannabis use helped modulate ADHD symptoms, particularly in the absence of other pharmacological treatments.37 Some people report cannabis is effective in improving attention and managing internal restlessness – symptoms that may be particularly pronounced in unmedicated ADHD.38
Unlike with nicotine and illicit drugs, ADHD alone may not predict early initiation of alcohol use or increased use in young people.39 Despite this, research suggests that people with ADHD are also at higher risk of developing alcohol use disorder (AUD).40 Up to 43% of people with ADHD meet the criteria for AUD. It is also suggested that around 20% of adults with AUD also have ADHD, but the actual number is thought to be much higher, due to underdiagnosis of ADHD.41 Those with late diagnosis and intervention for ADHD are more likely to develop more serious problems with alcohol.42 The reasons for increased risk of AUD in people with ADHD symptomology could be linked to their shared genetic and neurobiological features. The self-medication hypothesis can also be applied to alcohol and ADHD; however, there is little research available on this topic.43
A link between ADHD symptomology and nicotine use has also been well established in literature. Young people with ADHD are more likely to initiate nicotine use than their neurotypical peers.44 Regular nicotine use and nicotine dependance are more common in people with ADHD in both youth and adulthood compared to neurotypical people.45 In fact, it is estimated that more than 40% of people with ADHD are habitual cigarette smokers.46 The connection between ADHD and nicotine use has also been posited to be a form of self-medication for unmanaged symptoms, as nicotine increases the availability of dopamine in the brain.40
Some of the symptoms of unmanaged or poorly managed ADHD also predispose individuals to initiating smoking cigarettes and may make it more difficult to stop. Positively, ADHD medication, particularly as an early intervention, reduces the risk of early smoking initiation in young people.47
People with ADHD may be more likely to have severe or complex SUD and greater difficulty in responding to interventions. As a result, treatment for SUD in adults with ADHD must consider the complexities of these comorbidities in order for people to respond effectively to interventions.48 To make the situation even more complex, up to 80% of people with ADHD also meet the criteria for one or more other psychiatric disorders, such as depression, anxiety, personality disorders or conduct disorders.49 This can make it more difficult to treat SUD in people with ADHD.
People with ADHD are more likely to have earlier onset of SUD, a higher likelihood of polydrug use and an increased risk of having concurrent SUDs (addiction to more than one type of substance). They are also more likely to have more hospitalisations and reported greater levels of suicidal behavior. People with ADHD are less likely to adhere to SUD treatment.50 Part of the difficulty in treating SUD in people with ADHD is that substances are often used to manage symptoms. Treatment for SUD alone is likely to be ineffective for patients with untreated or poorly managed ADHD. However, the effective treatment of ADHD often results in improvements in other comorbid conditions, including SUD.51
It may also be difficult to diagnose ADHD in people with active SUD, due to the overlapping symptomology of both conditions. There has been concern that, due to this, ADHD may be misdiagnosed in people with SUD. However, research has shown that in 95.3% of SUD patients that were diagnosed with ADHD, the diagnosis was later confirmed during periods of abstinence.52
Alongside medication, CBT and other psychotherapeutic approaches to SUD can be effective for people with ADHD.53 However, most of the current approaches to behavioural and therapeutic interventions for SUD have been developed for neurotypical individuals. People with ADHD take longer to achieve recovery or stabilisation in SUD than neurotypical people, which is not accounted for in traditional alcohol and other drug (AOD) interventions.54 It is important to consider that people with ADHD may have different needs and more challenging presentations of SUD. Clinicians and AOD services must consider what services are most appropriate; these may be different to what is recommended for neurotypical individuals.
Internationally, there still appears to be reluctance within some medical communities to prescribe stimulant medication to individuals with SUD. Concerns stem from the idea that people with SUD may be more likely to abuse or divert pharmaceutical stimulant medications. However, research does not support this theory. In fact, young people that are treated appropriately with stimulant medicines are less likely to develop SUD in their lifetimes than those who are not.55 Other meta-analyses have found that in the vast majority of studies, appropriate pharmacological treatment of ADHD is likely to reduce the risk of SUD across a person’s lifetime and should be considered a protective factor.56
Despite this, some prevailing medical perspectives still assert that pharmacological ADHD treatment should only be provided after SUD has been resolved. However, due to the difficulty in treating SUD when ADHD symptoms are unmanaged, this is not recommended as best practice and may actually inhibit a person’s ability to make positive progress in recovering from SUD.57 Where there are concerns that a person with co-occurring SUD and ADHD may misuse or divert medications, there are second-line treatments including long-acting stimulants (i.e., lisdexamfetamine) or non-stimulant treatments (i.e., atomoxetine) that can be offered that pose less risk of diversion and misuse. With appropriate clinical guidance and support, first-line stimulant treatment for ADHD is effective for most patients, even in the presence of a co-occurring SUD.58
If ADHD is screened for, diagnosed and treated early, it reduces the risk of developing substance use issues both in youth and later in life.59 Youth with ADHD that received appropriate and timely pharmacotherapy had an 85% reduction in risk for developing a SUD compared to those not receiving treatment.60 This statistic highlights how crucial it is that screening and diagnosis are accessible as widely as possible.
Research has been contradictory in the past regarding whether psychostimulant medication treatment for ADHD could lead to substance use and SUD later in life. Older literature had posited that psychostimulant treatment increased the risk of future substance use in ADHD individuals; however, this has since been largely disproven.61 More recent research has shown that prescription psychostimulants do not act as a ‘gateway’ for people with ADHD to access illicit substances or develop SUD.62 A meta-analytic literature review conducted by Wilens et al. attempted to answer the hypothesis that children/adolescents with ADHD receiving stimulant-based treatment may result in an increased risk for SUD in adulthood.63 Based on their analysis of the research, which included 674 medicated subjects and 360 unmedicated subjects (followed for four years), this hypothesis was disproved. The results suggested that when ADHD is correctly diagnosed in childhood/adolescence and effectively managed, the likelihood of developing SUDs is reduced. If a person does develop a SUD, effective treatment of ADHD results in better outcomes in the management of SUD.
Early diagnosis of ADHD also helps to ensure the right supports are in place to identify issues as they arise. Due to the common comorbidity of ADHD and other mental health and conduct disorders, this is particularly important. This also allows for the early engagement with harm reduction approaches if substance use issues develop. Harm reduction education and strategies appear to be effective in reducing drug-related harm for people with ADHD using substances.64
It is important to acknowledge that the risks of missed diagnosis of ADHD are broad. Untreated ADHD often results in increased risky behaviour, which can result in serious harm. Untreated ADHD has been linked to increased risk of motor vehicle accidents, risky sexual behaviour and imprisonment.65, 66, 67 People with ADHD and SUD are more likely to die early; this is particularly pronounced for people with untreated or unmanaged ADHD.68 Whilst there is little literature on this, it is likely that these risks are pronounced for more vulnerable groups such as Māori, people of colour and disabled people.
There is little evidence to suggest the existence of adult-onset ADHD.69 However, missed diagnosis in childhood is relatively common and diagnosis and screening of ADHD often misses people with atypical presentations and manifestations of ADHD.70 Missed ADHD diagnosis is also very common in women and girls.71 Beyond this, there are a plethora of reasons why an ADHD diagnosis may be missed in childhood or youth, including barriers to access for diagnosis (financial, social or structural) or misdiagnosis due to co-occurring mental illness. Due to this, it is recommended that all people with SUD seeking treatment be screened for ADHD.72 Despite concerns that it may be difficult to diagnose ADHD in people with active SUD, it is recommended that a pragmatic approach is taken to evaluate people for ADHD even where a person has not been abstinent.73 In the vast majority of cases, having an ADHD diagnosis helps the clinical approach to managing concurrent ADHD and SUD and results in better outcomes for individuals.
ASD and substance use
What is ASD?
Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with the world.74 Due to its generally early onset (first two years of life), it is considered a developmental disorder. ASD exists on a ‘spectrum,’ meaning that people experience it differently and have different types and severity of symptoms.75 There is wide variation in how symptoms of ASD present in different people.
ASD can affect a person’s ability to relate to others and can result in a person having difficulty adjusting their behaviour to social situations. People with ASD can find it difficult to interact with people and perceive social cues. ASD can also affect a person’s ability to adjust to changes in their environment and result in an increased likelihood of feeling overwhelmed or overstimulated. People with ASD may also be hypersensitive to certain stimuli in their environment and can find it difficult to regulate sensory input.76
It has been posited that people with ASD may be at higher risk of using substances as a form of self-medicating for their symptoms. There is some research depicting the relationship between substance use and SUDs and AUDs. However, there is contradicting evidence on this topic, and a large number of gaps in our understanding of why people with ASD use drugs.
Takiwātanga is a Māori word used to describe autism. It means “in his/her/their own space and time”.77
There is a lack of consensus among researchers as to whether ASD is a risk factor for substance use. Adhia et al. (2020) analysed research on alcohol and cannabis use in individuals with ASD.78 They found that there was a significant lack of research in this area, despite the potential for people with ASD to be at increased risk of developing SUD. Another meta-analysis by Huxley (2018) found that studies on the correlation between those with intellectual disabilities and substance use were highly variable and heterogenous.79 Sample numbers were also often small, making it difficult to draw conclusions.
One posited relationship between ASD and substance use is that people with ASD may be more likely to use alcohol or other drugs as a tool for coping.
Livingston (2021) surveyed autistic and non-autistic individuals about their substance use.80 They found that autistic individuals were less likely to use alcohol or other drugs compared to neurotypical individuals. However, their qualitative research indicated that those individuals that did use alcohol or other drugs reportedly did so to “manage behaviour” or “cope with mental health”; these themes were less prevalent in non-autistic respondents. This identified a potential area of concern, as these motivations for use may be more likely to result in problematic or dependent substance use behaviours. Further research has also shown that people with ASD are more likely to report drinking alcohol as a coping mechanism or for social anxiety, compared to those without ASD.81
A 2021 study found that substance use in people with diagnosed ASD was estimated at 16% compared to 22% of neurotypical adults.82 However, this study found that adults diagnosed with ASD were nine times more likely to use drugs to manage ‘unwanted symptoms’ associated with ASD. Adults with ASD were also three times more likely to use substances to manage mental health symptoms, including anxiety, depression and suicidal thoughts. People with ASD reported some utility for substance use in effectively managing symptoms, reducing sensory overload, or supporting in social ‘masking’.
The most prevalent theme in the research on ASD and substance use is that it is difficult to understand the relationship between the two. Research done on these groups is often conducted with methods developed for neurotypical individuals. There is also the obvious problem of underdiagnosis of ASD, especially in women, people of colour and people with co-occurring disabilities. The majority of studies recruit individuals who have a current ASD diagnosis. This has likely resulted in underrepresentation of many people with ASD in research.
82. Weir, E, Allison, C, & Baron-Cohen, S. Understanding the substance use of autistic adolescents and adults: a mixed methods approach. The Lancet Psychiatry (2021).
Historically, research has suggested that SUD is lower in populations of people with ASD compared to neurotypical people. A meta-analysis of 18 papers that looked at ASD and SUD found that, generally, SUD was lower in the associated ASD populations examined.83 However, they also indicated that most research was conducted in treatment populations, which makes it difficult to establish whether people with ASD are less likely to have SUD, or simply less likely to access treatment. Overall, the range of SUD occurrence in people with ASD is large.84
Some studies claim the incidence could be as high as a 36% – much larger than the overall estimate of a 12.3% lifetime prevalence of SUD in New Zealand.85
Some research has outlined that ASD may be a risk factor for developing SUD. A study of over 6,000 people with ASD described a link between ASD and the development of SUD in people who initiated substance use.86 The researchers found that people with ASD were at greater risk of mortality from overdose compared to those without ASD. Another study found that the risk factors for SUD in people with ASD were six times higher than those of neurotypical people.87 Regardless of the actual incidence of SUD in people with ASD, it is clear that SUD may impact these individuals more severely than neurotypical people.88 On top of this, people with ASD often have fewer protective factors for managing problematic substance use behaviours, including strong social support.
Low mood in people with ASD may also be a motivator for engaging in substance use.89 Self-medication of mental health symptoms associated with ASD can lead to worsening issues over time. Further, using substances for managing mental health symptoms presents a higher risk of escalating into problematic substance use or SUD. Individuals diagnosed with ASD were also four times more likely to report vulnerability and risk associated with substance use compared to neurotypical individuals.90
One theory as to why there is increased risk of SUD for people with ASD is due to the co-occurrence of ASD and other mental health diagnoses, such as anxiety or depression.91 There is a complex intersection between ASD, mental illness and SUD,92 which is not fully understood in the literature. However, it is well established that the co-occurrence of ASD and mental health conditions such as anxiety or depression is a risk factor for problematic substance use.
90. Weir, E, Allison, C, & Baron-Cohen, S. Understanding the substance use of autistic adolescents and adults: a mixed methods approach. The Lancet Psychiatry (2021).
The common screening tools for SUD diagnosis are often not fit for purpose for people with ASD. One study outlined that indicative scoring on the DSMV questions for substance use indicates an ASSIST screening tool to be used for assessing SUD. However, this tool assumes neurotypical experiences to assess a person’s ‘baseline’ before their substance use, which may not relate to people with ASD. Other screening tools rely on a person’s ability to assess the impact of their substance use on others, which can be challenging for some people with ASD.93
This study also suggests that face-to-face screening for SUD may be challenging for people with ASD.
Equally, online tools may not provide clear instruction and make it difficult for people to self-assess. Whatever screening tools are used, it is important that clinicians are aware of the possible difficulties in assessing substance use in people with ASD.
Other research has found that there does not appear to be clinical consensus about the best way to screen for SUD in people with ASD. Diagnosis can be challenging across many different screening tools.94 Unlike with other psychiatric and mental health conditions, SUD is not often routinely screened for in people with ASD.95 To add to this, SUD symptoms may manifest or present differently in people with ASD.96 All of these things can make diagnosis of SUD in people with ASD much more complex and can result in missed diagnosis.
Evidence shows that people with ASD and SUD may have a harder time accessing AOD treatment and intervention. They may also have higher attrition from SUD interventions/rehabilitation than neurotypical people. One study found that the available treatments for SUD respond to the needs of neurotypical individuals and are often not appropriate for people with ASD.97 Due to this, studies on ASD and SUD in traditional treatment facilities are likely to not represent this population as a whole.
Access to, and uptake of addiction treatment in people with ASD is low.98 People with ASD are likely to have many more barriers to SUD treatment compared to neurotypical people. Barriers can include perceived and experienced stigma and lack of tailored services.99 During treatment, people with ASD may also drop out due to ASD-related stressors in their lives as well as sensory overload in treatment settings.100
Medication assisted treatment (MAT) may also work differently for people with ASD, including opioid substitution therapy (OST).101 There is little research on the tolerance of MAT in people with ASD. It is theorised that it is possible people with ASD would experience more sedating effects from OST or benzodiazepine MAT medicines, which is important to consider in treatment planning.102 Currently there are no specific guidelines for prescribing MAT or other associated medicines for managing SUD in people with ASD. This can make SUD treatment complex for patients and clinicians alike.
Individuals with ASD are also at a potential greater risk of substance-related death than those without ASD. One study found that people with ASD were significantly more likely to die as a result of substance use, even when factors of education, age and familial income were mediated for.103
Research has suggested that there has been an increase in individuals using CBD and THC products for the treatment of ASD-related symptoms.104 Other evidence suggests that THC and CBD use may increase the risk of developing symptoms such as psychosis, irritability and loss of appetite in individuals with ASD.
Another study examined the relationship between ASD and cannabis use. The authors found that cannabis offered therapeutic improvement in several aspects of life for people with ASD, such as reducing anxiety, irritability, restlessness, aggression and depression.105 Due to the benefits of cannabis on ASD, it is very conceivable that people may seek out cannabis illicitly where it is medicinally inaccessible, as a means of self-medicating.
Online discussions of ASD and cannabis use include self-reports of using cannabis to cope with symptoms of neurodivergence. One online forum thread includes individual experiences of cannabis helping them focus on school or work and reducing the overall negative symptoms associated with ASD.106 Some people also shared their negative experiences with using cannabis to address ASD symptoms, including finding it easy to ‘abuse’, having issues with memory and it reducing their ability to ‘mask’ in social situations. A quick review of these personal experiences online shows that the benefits of cannabis can be significant for some individuals with ASD. Overwhelmingly, the personal reports discuss the utility of cannabis as a coping mechanism, rather than something that is used for recreational purposes.
Research has indicated a possible link between ASD and alcohol use disorders (AUD). One study found that alcohol dependence occurred in 35% of people surveyed with ASD, compared to 20% of those without ASD.107 Another study found that alcohol use traits in people with ASD occurred in a ‘U’ shape. Non-drinking and hazardous drinking were both more likely to occur in people with ASD compared to non-hazardous drinking.108 This finding fits with what we understand of ASD and substance use behaviours in general.
Despite this research, there is not a consensus about the risk of hazardous drinking in people with ASD. Other studies suggest that people with ASD may be less likely to engage in risky drinking behaviours compared to neurotypical individuals.109
Overall, there is not sufficient information on understanding the risk of hazardous drinking in people with ASD, particularly in youth and adolescence.110 There may be many reasons why people with ASD engage in hazardous drinking. One study posited that alcohol may be used as a form of selfmedication to help alleviate some of the stressors (particularly social stressors) in people with ASD.111 The study also found that alcohol use in people with ASD may be affected by sensory processing issues, including how it affects the sensory experiences of people with ASD.
In Aotearoa New Zealand data on both ADHD and ASD is not effectively captured; we rely on estimates to understand the national prevalence of these neurodivergences. One New Zealand study found that 0.6% of the adult population was receiving ADHD pharmacological treatment.112 However, the actual estimate of ADHD prevalence in adults is 2.6%, suggesting that our prescribing data does not reflect the actual number of individuals with ADHD in New Zealand. This research also showed that Māori are more likely to be under-prescribed ADHD medication, making up only 10% of people receiving pharmacological treatment, despite being 17% of the total New Zealand population.
Further, 2020 data from the Ministry of Health suggests that only 2.4% of people reported an ADHD diagnosis.113 However, Australian data suggests that the prevalence of ADHD is estimated to be 6–10% of children and adolescents, and 2–6% of adults.114 Worldwide, the estimates of ADHD prevalence have increased over the last decade. This is likely not due to a greater actual prevalence of ADHD, but rather increased access to diagnosis and more inclusive diagnostic criteria. Increases in prevalence also likely represent better diagnosis of ADHD in previously underdiagnosed populations, such as adults and women and girls. A recent American study found that ADHD diagnosis in adulthood has increased by 123% over the last 10 years.115
In New Zealand, it is difficult to obtain an ADHD diagnosis, particularly for adults.116 Children and adolescents can be diagnosed by a pediatrician or psychiatrist. Childhood diagnoses are more accessible via the public health system than they are for adults — but wait times can still be significant. For adults, ADHD can be diagnosed by a psychiatrist; it can also be diagnosed by a clinical psychologist, but they are not able to prescribe pharmacological treatment. The public health diagnostic system for adult ADHD is significantly inaccessible – being described by some as “virtually impossible” to obtain an appointment.117 Assessments by private psychiatrists in New Zealand are the most effective means of obtaining a diagnosis; however, these are costly and wait times are often several months, and in some cases over a year. A survey by ADHD New Zealand found that 33% of people who received a referral for ADHD assessment had given up waiting for an appointment with a psychiatrist.118
Due to underdiagnosis, it is very likely that approximations of ADHD prevalence in New Zealand, particularly in adults, are underestimating the actual numbers.
The majority of New Zealand research on ASD prevalence is focused on diagnosis in children. One study found that ASD diagnoses for children in New Zealand were made in 1.48 per 1,000 people aged 0–9.119 Of these diagnoses, 87.4% occurred under the age of nine. Another study found that the identification rate for ASD in eight-year-old New Zealanders was one in 102.120 Both studies found that ASD diagnoses were approximately four times more common in males compared to females.
International research suggests that ASD prevalence is higher than these New Zealand findings. Estimates range from one in 54 to one in 66 children diagnosed with ASD.121 The estimated prevalence of ASD in New Zealand may be undercounted by as much as 40%.122 International research corroborates the findings that males are diagnosed with ASD considerably more than females.
In New Zealand, assessing a child for ASD usually starts with a referral from a GP and a diagnosis by a developmental pediatrician within the public system.123 Waiting lists for childhood ASD diagnosis in New Zealand can be several months and not all referrals are accepted. However, it is considerably easier to get a diagnosis for ASD in early childhood compared to later in life. ASD may also be diagnosed by qualified psychologists or psychiatrists via the private healthcare system.
For adults, accessing an ASD diagnosis is much more difficult. Public system referrals for adults with ASD are very rare, and a person is unlikely to receive an appointment unless they have severe mental illness or significant intellectual disability.124 Referrals to qualified private psychiatrists or psychologists are often the only option for adults seeking a diagnosis. Private appointments are costly and wait times can be long. Despite this, research has shown that adults with ASD in New Zealand report satisfaction with the diagnostic assessment stages. Unfortunately, they also report marked dissatisfaction with post-diagnostic support and report many unmet needs related to their diagnosis.125
There are some pharmacological treatments for ASD, but their efficacy remains largely up for debate.126 Clinical guidance in New Zealand suggests that prescribing for ASD should be focused on identifying and relieving co-occurring mental health conditions or ADHD;127 however, these treatments are unlikely to affect the difficulties associated with the core characteristics of ASD. People with undiagnosed ASD may be less likely to receive appropriate pharmacological treatment for co-occurring mental health conditions.
Drug use and harm is a persistent problem in Aotearoa New Zealand. New Zealand has comparably high levels of stimulant use to other parts of the world, particularly in the use of methamphetamine. New Zealand is in the top five countries worldwide in the consumption of methamphetamine per capita.128 The highest levels of methamphetamine use across the country are often in our poorest areas.129 Despite these high levels of methamphetamine use, it is important to note that the 2012/13 New Zealand Health Survey showed that 78% of people who used amphetamine drugs used them less than monthly.
Aotearoa New Zealand has also seen an increase in drug-related deaths. Between 2016 and 2023, 1,179 people died of accidental drug overdose.130 Concerningly, deaths from overdoses have increased over the last few years. These overdose deaths only account for acute overdoses and do not include deaths resulting in chronic harm from the use of drugs and alcohol. The health burden of the chronic effects of drug use and SUD are significant, both nationally and internationally.131
Despite growing concerns associated with increased drug use and harm in Aotearoa New Zealand, our mental health and addictions services have not significantly increased to respond to the need. A report from 2020/21 found that wait times for accessing addiction services had increased from five years prior.132 There also remains a lack of services supporting people who are not at the high end of harm from substances, including non-abstinence harm reduction support, peer-support services and low-threshold community treatment options.
The burden of lack of access to diagnosis and treatment for ASD and ADHD and support for substance use disproportionately impacts some communities. Māori have continually faced drug-related inequities, ultimately being three times more likely to die from drug-related deaths than non-Māori.133 Māori are also 1.8 times more likely to use amphetamines, including methamphetamine, compared to non-Māori. It is also thought that the underdiagnosis of ASD and ADHD disproportionately impacts Māori. Inequities in our healthcare system, including in mental health and addictions services, widen the gap in inequity for Māori and often result in poorer overall health outcomes.134 There is very little research on the intersectionality of SUD and neurodivergence for Māori; this is urgently needed to better understand what can be done to improve outcomes.
Both the number of diagnoses of ADHD and ASD and the incidence of substance use disorders and substance use harm have increased over the last decade.135, 136, 137 This has resulted in challenges for traditional mental health and addiction services, particularly in responding to the unique needs of neurodivergent people with SUDs. Despite the growing number of neurodivergent people experiencing harm from substance use, there are some fantastic examples from across the globe of health systems working to innovatively address these needs.
New clinical guidance for diagnosing ADHD that recognises the complexities of diagnosis in atypical groups is a promising development. For example, The Australasian ADHD Professionals Association (AADPA) has released new clinical guidelines for screening, assessing and diagnosing ADHD. These guidelines are working to bridge existing gaps for adult diagnosis and diagnosis of other groups that are less likely to receive early intervention (i.e., girls and women). Although comprehensive, these guidelines provide a very straightforward set of recommendations for clinicians.138
The guidelines provide a list of groups of people who are considered high risk for ADHD; this is comprehensive and identifies groups that may otherwise be missed by traditional screening practices. The guidelines recommend best-practice screening processes for health professionals and emphasise the importance of assessment of co-occurring conditions. The guidelines discuss multi-modal treatment practices, including pharmaceutical, behavioural and psychological interventions, as well as management considerations for specific groups.
Similarly, the American Professional Society of ADHD and Related Disorders (APSARD) is releasing diagnostic and treatment guidelines for ADHD in adults this year (2024). Guidance focused specifically on adult ADHD may help to support those self-medicating with substances as a result of SUD.
Traditional SUD interventions may not be appropriate or effective for neurodivergent people. As an alternative, there has been an increase in the availability of community-based support services that offer promising alternatives for neurodivergent people.
In Aotearoa New Zealand, Speed Freaks is a peer-based charity organisation that focuses on walking and running groups to empower people on a journey to recovering from SUD and mental illness. These groups promote a safe environment, community, a physical outlet and an important sense of belonging.139 Instead of traditional models for SUD peer support (such as Alcoholics/Narcotics Anonymous), Speed Freaks centre peer connection and community on physical movement.
For neurodivergent people, particularly those with ADHD, exercise has been proven to support functional outcomes.140 The physical aspect of the Speed Freaks model helps people to regulate symptoms they may have otherwise self-medicated with drugs or alcohol. Whilst Speed Freaks is open to anyone, they have a special focus on offering alternative support for people with ADHD and other neurodiverse conditions, and have many members with lived experience.
More generally, research is showing that peer-led models for communitybased programmes are bridging gaps left by traditional treatment services for people with a range of disabilities. A 2022 study found that peerinitiated programmes were very successful in overcoming existing barriers to SUD treatment for people with an array of disabilities.141
There are also some promising examples of services working towards creating adaptive AOD interventions for people with neurodivergent conditions. Due to the complexities of the intersectionality between ADHD/ ASD and SUD, effective support must take into consideration the unique needs of these groups.
Addictions UK is working to create adaptive AOD services across the UK for neurodivergent people.142
They have proposed four projects that aim to enhance support access and improve experiences for this group, namely:
- A welfare rights and legal service for those with addiction and neurodivergent conditions.
- A research project to expand and disseminate knowledge about the connection between neurodiversity and addiction.
- An online resource for neurodiverse people with addictions that allows for communication, collaboration and mutual-aid support.
- Training for addictions and health professionals on the complex relationship between neurodiversity and SUD, and how to better diagnose and manage people with these comorbidities.
If realised, these proposed projects are promising and could significantly impact the way that neurodivergence is treated within addiction services across the UK.
Equally, there has been more research done recently on the importance of adapting SUD treatment models to work for people with ASD and ADHD. A 2022 study found that CBT group treatment that is tailored specifically for people with ASD was effective in improving symptoms of both ASD and SUD.143 This adapted treatment focused on increasing the sense of control in patients with co-occurring ASD and SUD. It also focused on getting participants to generalise the interventions from CBT into their daily life, which can sometimes be difficult for people with ASD. By recognising the unique experiences of people with ASD, adapted CBT was effective in mitigating problems from substance use.
There do not always need to be new services developed to address the needs of neurodivergent people with SUD. Recent research focused on providing regular education to therapists and health workers at a traditional SUD support service to increase their competence in understanding of ASD.144 Regular education and group supervision for these workers was shown to improve the outcomes for their patients with ASD. This research also recognised that patients with co-occurring ASD and SUD needed more support sessions compared to neurotypical patients, and therapy needed to be more direct and individualised. Patients also benefited from more general support in socialisation, understanding their ASD, and support in coordinating other aspects of their lives (i.e., social assistance, housing, medical care).
There has also been research focused on specific SUD interventions for people with ADHD. Tailored support models for treatment are most effective for those with co-occurring ADHD and SUD.145 Interventions such as adapted structured skill training programmes may be effective supports for people with ADHD.146
Common clinical guidance has long suggested that psychostimulant ADHD medicines are not prescribed to people experiencing active SUD, due to the risk of misuse or diversion of these substances.147 This process involves a person having to reach a period of stabilisation in their substance use (usually predicated on full abstinence) before being assessed and treated for ADHD.148 Historically, this has been the stance of much of the literature around ADHD and SUD.
Despite these concerns, there is little actual evidence to suggest that prescribing ADHD pharmacotherapy to people with SUD results in the misuse or diversion of these medicines.149 The more common issues for treating ADHD in people with SUD are related to possible increased tolerance to these medicines if using illicit stimulants. If the person is still actively using substances there is also an increased risk of harm from the combination of these with prescribed psychostimulants, but this can be managed clinically.150 Rather than misusing or diverting these medicines, this research suggests that people with comorbid ADHD and SUD may have greater difficulty with medication adherence.
Overall, current evidence suggests that to increase success of stabilisation or recovery for people with concurrent SUD and ADHD, it is imperative that ADHD symptoms are treated simultaneously.143 The majority of clinicians are in agreement that treating ADHD supports a person’s ability to manage their SUD and often aids in longer-term recovery.151 Withholding pharmacotherapy from people can have adverse effects and ultimately result in greater harm for the individual. There are alternative options for psychostimulant treatment that are less likely to be misused, where there is genuine concern, including extended-release preparations, such as lisdexamfetamine.
However, it must be stated that it can be difficult to diagnose ADHD when there is a concurrent, active SUD.152 This is especially the case when the SUD is severe. Active SUD and ADHD can share many similar characteristics, and long-term use of substances can result in the development of ADHD-like symptoms. For this reason, taking novel approaches to managing people with SUD and ADHD symptoms is imperative.
More recently, there has been progress made in stimulant substitution therapy (SST) for people with stimulant use disorders. SST is a form of medication assisted treatment (MAT), where a medication with similar effects to an illicit drug is used to relieve cravings and minimise harms caused by illicit drugs. The most prominent example of MAT is opioid substitution therapy (OST), where opioid agonists (i.e., methadone) are used to treat people with opioid use disorder.
In Canada, there has been an emergence of pilot studies that show promising insights into the success of SST.153 These interventions use common ADHD pharmacotherapies — methylphenidate and dexamphetamine to titrate people off illicit stimulants such as cocaine or methamphetamine. Due to the considerable number of people with ADHD who have a concurrent stimulant use disorder, it is thought that SST may increase the likelihood of recovery in undiagnosed individuals. Importantly, these SST practices don’t rely on a person first receiving an ADHD diagnosis, as this process can be complex when someone has severe SUD.
Additionally, an Australian study is currently investigating the use of lisdexamfetamine (extended-release ADHD pharmacotherapy) as a replacement for those with methamphetamine dependence.154 The product, called Vyvanse, is formulated as delayed release, and can only be metabolised through digestive processes. This reduces the misuse potential of the medicine, making wider access to it more feasible. Although ongoing, this study evidences that lisdexamfetamine could be highly beneficial regarding both harm reduction for illicit stimulant use and co-occurring ADHD.
Community experiences
To contextualise the findings of our literature summary, we wanted to understand the unique perspectives of people with living experience of ADHD and/or ASD and substance use. In the absence of being able to conduct formal research on this topic, the Drug Foundation held group and one-to-one conversations with people connected with the organisation to discuss their personal and professional experiences of neurodivergence and substance use.
These conversations revealed that peoples’ experiences were often in line with what we found in the literature. Prominent themes emerged, including using substances to self-medicate, experiences of problematic substance use, difficulty obtaining diagnosis, physical and mental comorbidities, and stigma within health and social care systems. Those receiving appropriate psychotherapeutic and/or pharmacological treatment shared significant improvements to substance use behaviors and overall wellbeing and quality of life.
We acknowledge the valuable input of these individuals as part of this report and the importance of including diverse perspectives from an Aotearoa New Zealand context. We hope in future to see qualitative academic research on this topic to bolster the findings of this report.
Our process
Over the period of a few months, we engaged with individuals and organisations that have insights and lived experience of ASD and/or ADHD and substance use. We asked a variety of structured questions focused on diagnosis and treatment of neurodivergence, substance use, and experiences with AOD interventions and wider health services.
The answers and insights from these engagements were summarised into key themes, which we have used to inform the recommendations in section 3.
Although incredibly valuable, these insights are not representative of all people with neurodivergence and substance use. We accept that there is a natural sampling bias, as we only surveyed a small number of people already engaged with the New Zealand Drug Foundation.
Summary of findings
These insights affirmed a connection between neurodivergence and substance use. This connection proved multifaceted, highlighting the heterogeneity of diverse, individual experience. We found all individuals with neurodivergent conditions faced significant challenges in receiving both diagnosis and support. Co-occurring mental health conditions were present in all individuals, which complicated the diagnostic process further.
Individuals and organisations spoke to the limits of the health system in Aotearoa New Zealand for those with neurodivergence and a history of substance use or SUD.
Findings & insights
Neurodivergence diagnosis and presentation
Half of the participants with lived experience had been diagnosed with ADHD as an adult, and the other half were self-diagnosed with ADHD and experiencing active symptoms; most of the latter had started the process to obtain a diagnosis. A few participants also had formally diagnosed ASD or reported ASD symptoms. Organisation representatives we spoke to worked closely with those with neurodivergence and substance use problems.
Issues highlighted were wait times, cost, stigma and system navigation as barriers. One individual was told to “come back next year” when seeking advice about a potential diagnosis, because current wait times were too long.
These symptoms included difficulty regulating emotion and concentration, sensory sensitivities, and general difficulties with communication and social settings. All participants had co-occurring mental and/or physical conditions, most commonly anxiety, depression, and PTSD. Most said these co-occurrences created further barriers to diagnosis and support, contributing to experiences of “not being taken seriously” or, in some cases, misdiagnosis.
Those formally diagnosed with ADHD were all medicated with prescription psychostimulants. Other prescription medications for co-occurring mental and physical conditions were typical and atypical anti-depressants/anti-anxieties, opioids, anti-psychotics, benzodiazepines and prescription cannabis.
Substance use was primarily attributed to self-medication and coping in these individuals. While some participants said that they also used substances for recreation, the majority of regular use was to manage challenging symptoms of ADHD and/or ASD. A common substance for managing symptoms was cannabis — several participants reported weekly or daily use. Other participants used mushrooms, opioids, stimulants and benzodiazepines.
A few participants considered themselves as being in active addiction or had a previous diagnosis of SUD. Almost all participants knew of someone in their life that had a neurodivergent condition and problematic substance use or addiction. Generally, participants felt that access to pharmaceutical treatment for their neurodivergence (particularly for ADHD) would reduce or completely eliminate their use of illicit substances. Substance use and dependence is an evident lived reality for many with neurodivergence.
According to the literature, health system experiences (including AOD sectors and medical care) are key to understanding why those with neurodivergent conditions are not receiving adequate support. Predictably, no one we spoke to had had a satisfactory, fulfilling or efficient experience with the healthcare sector in Aotearoa New Zealand.
People felt that there was a general lack of cohesion and centralisation of support services for those diagnosed with a neurodivergent condition, particularly for ADHD. Once diagnosed, people felt it was the responsibility of themselves and their family to manage this. Outside of pharmacotherapy, participants did not report any proactive support options to help manage their condition.
Participants shared that they felt feelings of mistrust from the health services they accessed. Some reflected on their experiences of being labelled as a ‘drug seeker’ when attempting to access diagnosis for neurodivergence (particularly ADHD). Other participants felt that when they disclosed their illicit substance use, this became a barrier to treatment.
Participants also shared that they felt unsafe sharing their illicit substance use with clinicians for fear of this impacting their ability to access treatment for both neurodivergence and other mental and physical health conditions. Some participants had been told outright by health professionals that they would not be able to be treated with ADHD psychostimulants due to their history with substance use, despite this not reflecting the actual prescribing regulations.155
Importantly, receiving a diagnosis of ADHD or ASD, with or without pharmacotherapy treatment, was related to positive outcomes for individuals.
Themes of finding a “sense of self through diagnosis”, understanding oneself in a different light and, importantly, enhancing networking with others who share similar diagnosis were common in participants. Many reported feeling validated in their experiences after receiving a diagnosis. Interventions including CBT, other therapy, lifestyle changes and medication were also described as essential.
Psychostimulant medicines for ADHD were described as the only thing that kept some participants functioning. People on pharmacotherapy for ADHD reported significant improvements in overall functioning and mental wellbeing. Participants reflected on life before and after diagnosis and treatment, highlighting the significant improvement in their overall quality of life and wellbeing.
Participants who were yet to receive formal diagnosis still found that understanding their symptoms as a product of neurodivergence was a positive experience. This process also helped people to make sense of their behaviours and coping mechanisms, including the use of substances to self-medicate. This reflexive practice was an important first step for all participants in acknowledging how their neurodivergence affected they way they experienced the world around them.
One of the most prominent themes that emerged across both living experience and organisational participants was a consensus on the vital role diagnosis plays in providing necessary support and fostering overall wellbeing. Pharmacotherapy, therapeutic interventions (i.e., CBT) and support in implementing lifestyle changes were all agreed to be essential for those with neurodivergent conditions.
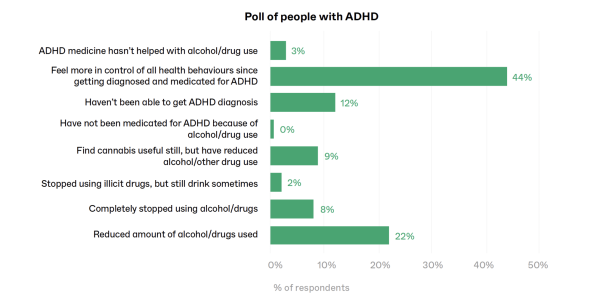
Further to the interviews conducted, an informal peer poll was run on the ADHD NZ community for adults with ADHD Facebook page by a Drug Foundation staff member. The poll was moderated by ADHD NZ. There were 582 responses to this poll and participants were able to choose more than one answer. The question and response choices were as follows:
“Which of the following applied to you once you were diagnosed and medicated for ADHD?”
- I was able to reduce the amount of alcohol/illicit drugs I use, or I use them in a less risky way
- I completely stopped using alcohol and other drugs
- I stopped using other illicit drugs, but I still drink sometimes
- I find cannabis useful still, but otherwise have reduced my alcohol/drug use
- I haven’t been able to get medicated for ADHD because of my alcohol/drug use
- I haven’t been able to get an ADHD diagnosis (e.g., I can’t afford it)
- I feel more in control of all health behaviours (drinking, drugs, food, nicotine, gambling, etc.) since getting diagnosed and medicated for ADHD
- ADHD medicine hasn’t helped me with alcohol/drug use
Almost half of the respondents reported feeling more in control of a variety of their behaviours, including alcohol and drug use. Almost a quarter of people responded that they were able to reduce the amount of alcohol and drugs they were using or use in a less risky way. Given respondents were providing answers from their personal Facebook accounts, it is possible that some people did not feel comfortable discussing their AOD use, so actual numbers may differ if done in an anonymised survey.
Recommendations
1. Streamline screening of ADHD in individuals with SUD or substance harm
Due to the common co-occurrence of ADHD and SUD, ensuring accessibility of low-barrier, integrated ADHD screening in health services is imperative.
This includes screening through AOD services, mental health services and residential AOD treatment and detox. Screening in other settings where high-risk individuals may present, such as prisons or corrections facilities, is also recommended. It is important that screening occurs early in engagement with an individual to ensure this is factored into their treatment plan.
2. Increase access to ADHD diagnosis
The current diagnostic process for ADHD is heavily privatised.
More resource needs to be put into bolstering the public diagnosis capacity, so that direct referrals from low-barrier screening services can be made. Preferably, a system change whereby patients could be diagnosed and treated by specialised/authorised general practitioners rather than psychiatrists would ease the burden on the current systems and allow for better-integrated management of comorbidities. However, it is important to note that this may not be a complete solution, particularly for groups such as people from low socio-economic backgrounds, Māori, Pacific peoples and disabled individuals.
3. Introduce clinical guidelines for screening, diagnosis and management of ADHD and ASD in adults
Missed diagnosis of ASD or ADHD in childhood is common. This is in part due to the diagnostic criteria for these conditions being heavily oriented around childhood presentations.
New Zealand should consider creating new guidance for the diagnosis of neurodivergent conditions in adulthood, focusing on the complications of comorbid conditions, including SUD and mental illness. Developing clinical guidelines similar to the recent work by AADPA would be beneficial.156
4. Tailor treatment approaches in the AOD sector for those with neurodivergence
Many AOD services in Aotearoa New Zealand do not provide tailored treatment for people with ADHD or ASD, despite this being imperative for effective support.
Tailored AOD support and intervention options across New Zealand would greatly increase the success of these programmes for neurodivergent individuals.
5. Offer training on neurodivergence and substance use for the addiction workforce
It is imperative that AOD clinicians and health workers understand the unique relationship between SUD and neurodivergence.
Regular education opportunities for the addictions workforce to learn about this is imperative in improving the experience of neurodivergent people accessing services. Education modules that can be accessed by health professionals could help bridge this gap in knowledge and reduce stigma.
6. Enhance community-based support
More dedicated funding is needed for on-the-ground community-led and peer-based support services for people with neurodivergence and SUD.
These groups are high value for cost and provide important social and community networks and connection for people. Community-based AOD supports may be even more important for people with ADHD and/or ASD as they are more likely to be flexible to their needs.
7. Ensure approaches to neurodiversity and substance use are equitable, culturally safe and work for Māori
It is important that all approaches to addressing ADHD and ASD and substance use – including screening, diagnosis, support and treatment – consider the unique needs of Māori across a variety of different social and regional contexts and are informed by an intersectional approach.
8. Avoid requiring abstinence before providing ADHD pharmacotherapy in clients with SUD
In New Zealand it is possible to prescribe ADHD psychostimulant medication to persons with SUD.
Whilst this is often a slightly more involved process than prescribing to people without SUD, it is feasible. Access to extended-release preparations may be recommended as a first-line treatment where there is concern for misuse of these medicines.
It is vital to the successful support of people with co-occurring ADHD and SUD that ADHD is able to be treated and managed pharmacologically. Withholding psychostimulant medicine where there is no significant clinical reason to do so can hinder a person’s treatment significantly.
9. Fund and expand access to lisdexamfetamine
Lisdexamfetamine (Vyvanse) is a prodrug approved for the treatment of ADHD.157
Its extended-release formulation and the nature of it being a prodrug make it more difficult to use for the purpose of getting high; this also reduces its diversion potential. For this reason, lisdexamfetamine is thought to be a positive solution for prescribing to people with SUD and ADHD where there is a risk of misuse. The availability of lisdexamfetamine may also make it more feasible for prescribing of this medicine for ADHD to occur without special authority. A Pharmac application for Vyvanse was submitted in 2021. In September 2024, Pharmac opened public consultation on the funding proposal for lisdexamfetamine, closing September 26. We await further updates on this progress.
10. Trial novel approaches to harm reduction such as stimulant substitution therapy
Stimulant substitution therapy (SST) aims to improve health outcomes for those with addiction to stimulants, and reduce harms associated with the illicit drug market.
Illicit stimulant substances such as methamphetamine can be titrated off and substituted with first-line ADHD treatment such as dexamphetamine or methylphenidate. Importantly, access to SST should not be tied to formal diagnosis of ADHD, to reduce barriers.
11. Increase research on neurodivergence and substance use in Aotearoa New Zealand
Invest in research to collect data on co-occurring neurodivergent conditions, substance use and SUD in New Zealand.
Particular attention should be paid to Māori with neurodivergence and co-occurring substance use, as this is where the largest equity gap exists. This data can inform future policy and provide valuable evidence for how to approach these issues in an Aotearoa New Zealand context.
12. Tailor existing harm reduction approaches for those with neurodivergence
Services such as drug checking and needle exchanges are important harm reduction services for people who use drugs.
However, these may not always be tailored to people with neurodivergence, which can make these services inaccessible to some of these people. Implements such as having sensory spaces and providing information in ways more tailored to people with neurodivergence would make these services more accessible.
These recommendations offer several areas in which our health and social systems can improve the wellbeing of neurodivergent people who use drugs.
The proactive implementation of these recommendations is likely to have long-term benefits for our healthcare systems and reduce the economic burden of physical disease, chronic illness and mental illness. Most importantly, these recommendations represent important opportunities for change to reduce the stigma for neurodivergent people who use drugs in Aotearoa New Zealand. Neurodivergent people deserve equitable access to care, support and compassion that enhances their ability to live long, happy and healthy lives.
Recent news

Untreated ADHD leading to addiction and drug harm
A new report shows New Zealand’s failure to adequately diagnose and treat ADHD is likely leading to significant drug harm, including from alcohol and nicotine.

What researchers at University of Auckland are learning from giving people microdoses of LSD
‘Microdosing’ psychedelics involves taking small, repeated doses of a psychedelic drug. Researcher Robin Murphy talks us through the latest Auckland University microdosing study.
New report shows NZ loses three people a week to preventable overdose
New data shows that fatal overdoses are continuing to increase.